National Palliative Care Standards
National Palliative Care Standards 5th Edition (for Specialist Palliative Care Services)
The National Palliative Care Standards (Edition 5) have been updated following consultation with the palliative care community and other stakeholders. Much has changed within palliative care over the past decade, including expansion of the evidence base for clinical care, re-design of service delivery models of care to meet changing community expectations and needs, and changes to the language used to describe those we care for. Most importantly there is increasing recognition that caring for people who are approaching and reaching the end of life is everybody’s business – everybody in health, aged and social care has a role to play.
In alignment with the World Health Organisation definition, Palliative Care Australia defines palliative care in the contemporary Australian context as:
Palliative care is person and family-centred care provided for a person with an active, progressive, advanced disease, who has little or no prospect of cure and who is expected to die, and for whom the primary treatment goal is to optimise the quality of life. Palliative Care Australia considers that the following elements are integral to understanding this definition of palliative care:
- Palliative care should be strongly responsive to the needs, preferences and values of people, their families and carers. A person and family-centred approach to palliative care is based on effective communication, shared decision-making and personal autonomy.
- Palliative care should be available to all people living with an active, progressive, advanced disease, regardless of the diagnosis.
- Palliative care affirms life while recognising that dying is an inevitable part of life. This means that palliative care is provided during the time that the person is living with a life-limiting illness, but it is not directed at either bringing forward or delaying death.
The National Palliative Care Standards (the Standards) clearly articulate and promote a vision for compassionate and appropriate specialist palliative care. The Standards recognise the importance of care that is person-centred and age-appropriate. In particular they point to the requirement for specific attention to the needs of people who may be especially vulnerable or at risk. This may include, but is not limited to, Aboriginal and Torres Strait Islanders; asylum seekers; people who have experienced torture and trauma; people who are experiencing homelessness; people living with mental illness, intellectual disabilities or dementia; paediatric populations; people with unique clinical needs; people who are lesbian, gay, bisexual, of transgender experience and people with intersex characteristics (LGBTI), people from culturally and linguistically diverse (CALD) communities, or those experiencing other forms of social or economic disadvantage.
The Standards need to be relevant to those specialist palliative care services with a sole practitioner, as well as larger services that are more resourced with comprehensive research and teaching roles – and to everything in between. They are generally normative standards but also incorporate aspirational components to support those services with growing capacity and capability.
This 5th edition of the Standards has been developed to reflect the significant changes that have occurred since 2005 and to continue to support specialist palliative care services as they work to ensure that the people they service have access to the highest quality of care as they approach and reach the end of life.
- View the full version of The National Palliative Care Standards (5th edition)
- View The National Palliative Care Standards Factsheet
Development of the National Palliative Care Standards 5th Edition
PCA began the Standards revision process in 2013. At this time the palliative care community felt strongly that any revision to the Standards should be done carefully, with deep consideration and input from the sector, and in reference to current evidence to ensure the 5th edition of the Standards adequately reflect the evolution of palliative care. As such, PCA took the decision to recommence the review process when adequate resources could be allocated towards this important piece of work.
The revision of the Standards was recommenced in 2015 with the establishment of the Standards Review Group who have presided over the ongoing revision and consultation process. This panel of palliative care clinicians, researchers and executives closely examined the 4th edition of the Standards to identify their strengths, limitations, gaps and areas of duplication. This group developed the first draft for review.
There were two consultation rounds for the draft 5th edition of the Standards. Firstly feedback from PCAs National Policy Advisory Committee (NPAC), member organisations and affiliate members from May to August 2017.
The second round of consultation involved an online survey in September 2017, culminating in receipt of 55 responses from palliative care services known to the National Standards Assessment Program (NSAP), people or organisations with a vested interest in the Standards, and affiliated government bodies. Where necessary, additional specialised feedback was sought from experts in a particular area.
In summary, a rigorous and extensive consultation process has supported the development of the 5th edition of the Standards. PCA is grateful for the wide interest and input it has received in the revision process and hopes that you find value in the 5th edition of these Standards.
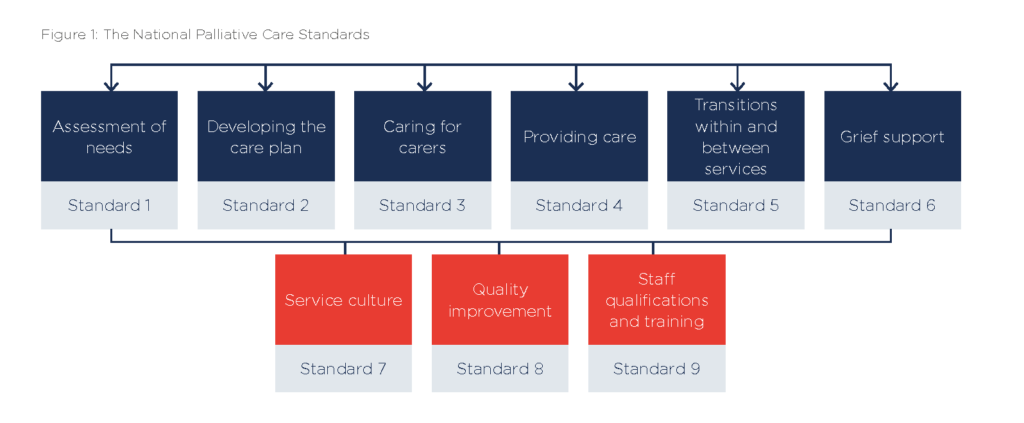
Mapping of the Standards
There is a growing number of standards that relate to the care of people approaching and reaching the end of life. Some are relevant to all services while others are specifically targeted at components of the health, aged and social care systems, for example aged care or acute care hospitals. These Standards are designed to complement other standards programmes. To assist services to identify these intersections and avoid duplication of effort, PCA have undertaken internal mapping of these Standards against standards of the agencies listed below:
- The Australian Commission on Safety and Quality in Health Care (ACSQHC) National Safety and Quality Health Service (NSQHS) Standards (Version 2).
- The ACSQHC National Consensus Statement:Essential Elements for Safe and High-Quality End-of-Life Care.
- The ACSQHC National Consensus Statement: Essential Elements for Safe and High-Quality Paediatric End-of-Life Care
- The Accreditation Standards, as identified in the Quality of Care Principles 2014 and administered by the Australian Aged Care Quality Agency (AACQA).
- The previous version of Palliative Care Australia’s Standards for Providing Quality Palliative Care for all Australians (2005).
PCA will continue to work with key stakeholders as newer versions of any relevant standards are released.
Acknowledgments
Palliative Care Australia (PCA) would like to acknowledge the people and organisations who contributed to developing the 5th edition of the National Palliative Care Standards (the Standards). Special thanks to the members of the Standards Review Group for their leadership and commitment in the review of the 2005 National Palliative Care Standards. Their contribution has been instrumental in creating standards that are based on the experiences of consumers, their carers and family; and which reflect concepts and principles to inform service delivery and development, as well as accreditation against other quality standards.
Standards Review Group
| Dr Meera Agar
Ingham Institute Applied Medical Research University Technology Sydney Mr Andrew Allsop (Chair) Silver Chain Hospice Care Service, WA Ms Liz Callaghan CEO, Palliative Care Australia Ms Kerri-Anne Dooley Home Instead Senior Care, Qld Dr Judi Greaves Palliative Care Researcher |
Ms Sue Hanson
Little Company of Mary Health Care Ltd A Prof Marianne Phillips Paediatric Palliative Care Australia & New Zealand and Princess Margaret Hospital for Children, WA Ms Claudia Virdun University Technology Sydney (UTS), NSW Ms Kate Weyman St Vincents Hospital, Sydney
|
Palliative Care Self Assessment online portal (PaCSA)
A continuous quality improvement program for palliative care services
Palliative Care Self Assessment (PaCSA) provides services with a secure online portal in which to self-assess against the National Palliative Care Standards (5th ed.), mapped against the National Safety and Quality Health Service Standards (2nd ed.), resulting in a quality improvement action plan.
For further information contact pacsa@palliativecare.org.au
See also: National Palliative Care Standards for All Health Professionals and Aged Care Services: for professionals not working in Specialist Palliative Care