The other half of palliative care
David Baxter was by his widowed mother's side in her bed when she died on 9 April 2020. She went as peacefully as possible, her head resting on David's shoulder. Her pain was under control, and she just stopped breathing whilst unconscious. One may think by reading these words that it was a proverbial "good death", but there is more to the story. David's mother, Betty, died in aged care in the early stages of the first wave of the COVID-19 pandemic.
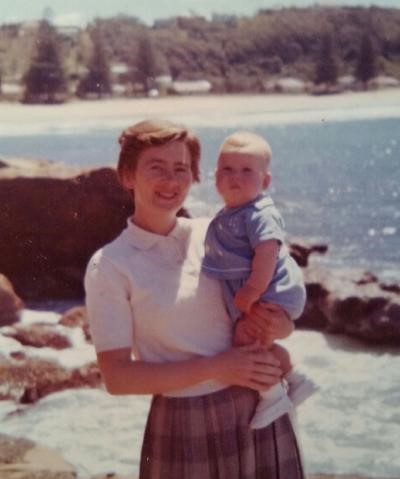
A caring and loving mother
Betty was born on 23 August 1929. Her father George was a bricklayer, her mother, Mona, kept the home, and her little brother, Robert, completed the close family. Betty was required to leave school when she was very young, before completing junior high school classes, to support her family with an extra income – owing to poverty flowing from and following the depression. Nonetheless, with her limited formal school education, she rose quickly with private studies and worked as a secretary for managers and executives in some large private companies. Her mathematics, English expression and spelling abilities, and her organisational skills were very highly regarded. Still, in that era, the positions were not very well paid and not very secure.
Betty married Don Baxter and lived together for over 50 years, until Don died on 23 December 2004 from a brain tumour. They were childhood sweethearts and adult soulmates. They played together in the local streets as children, played tennis and went on social outings as teens. Don was a first-grade goalkeeper and Betty – his biggest fan – was present at all games. Don held a job with the Australian Navy in civil stores for his entire working life.
Betty gave up her secretarial work when David was born on 15 April 1962, and she kept the home and cared for David until he started high school. During those years, Betty mended children’s clothing and was very involved in David’s school life. She participated in parent volunteer activities at his schools. From kindergarten through to the early years of primary school, David remembers his mother walking him to and from school every day. She always gave David unconditional love, with sensible guidance and bounds – as did Don. Betty highly valued education and supported and encouraged David. David was the first member of the family to attend University, completing a double degree in Economics and Law in 1985. Betty finished her working career as a teachers’ aid, using her skills to help children with learning difficulties to read.
Becoming a full-time carer
David believes that Betty began to show signs of material cognitive and physical decline from mid-2011 and was formally diagnosed with dementia in August 2013. Her condition was later diagnosed to solely Lewy Body Disease in November 2014. The characteristic symptoms and signs of that spectrum disorder became more prominent: dementia, movement disorders – similar to Parkinson's disease – and hallucinations. Betty also had a substantial and progressive loss of sight due to Glaucoma and had recurring skin cancers. To compound the loss of sight, she had a chronic tear-duct infection which required her eyes to be carefully cleaned twice daily.
David, an only child living alone with Betty, with no family of his own, decided to initially reduce his work hours to part-time to support in-home care services. Then, he ceased all work to be her full-time carer from April 2015, with continued support from additional in-home care services. Unfortunately, Betty remained on a waiting list for an approved high care aged care home care package, and most additional in-home care services were privately funded by David – who qualified only for a carer allowance. However, when the disease progressed to a stage where it was no longer safe for Betty to stay home and after one particularly bad accident, very fortunately with no lasting effects, she was moved to a residential aged care facility in September 2016.
By this stage, in addition to her dementia, Betty had lost any effective use of her legs, and one arm and hand, was doubly incontinent and had essentially lost her sight. However, her gentle and loving personality had thankfully been preserved. She enjoyed her music, food and treats and all company, and simple conversation that she could often understand and engage in with a big smile. David received a lot of advice from acquaintances that his role in Betty's care would now change, with some suggesting he only visited the residential aged care facility and not engage in further caring activities.
But David quickly appreciated the situation was different. He observed from the outset that her health, happiness, her ability to use her residual capacities and opportunities to present her loving and gentle personality – indeed her quality of life – was highly and positively correlated with his presence and Betty's awareness of his presence. His presence, voice and touch mattered.
"I found that with my Mum's move to the nursing home, only the location of my full-time care changed, but Mum had greater and more immediately available support services to supplement that care".
The care David provided is what he calls "the other half of palliative care". He talked to his mother, played her favourite music for her, sang songs with her, watched and regularly cleaned her eyes, monitored her skin and general health, and made sure she was comfortable in her room or on the balconies in fresh air. He fed her most of her meals at her own comfortable pace and her favourite sweets he brought each day. When Betty had trouble eating or was clearly not herself and possibly unwell, David quickly alerted staff and explained the symptoms and signs to the attending general practitioner, speech pathologists, and physiotherapists as Betty could not. He also went by himself to see her treating specialists (eye, skin and geriatric) periodically to discuss her condition and relay their recommendations.
“According to the Government through Centrelink, when someone is in a nursing home, their needs are fully looked after. It is, sadly, not the case. The fact is that it would simply not be commercially viable for aged care homes to provide the care that I was providing. I attended the nursing home every day, for an average – with little variation – of twelve hours; leaving at around 10.30 pm with Betty asleep to return to the family home overnight.”
The government's policy meant that he would no longer receive a carer's allowance despite caring for his mother full-time.
"A full-time carer providing that service to a family member in a nursing home receives no benefit. I received no wage or social security benefits, but my job was simply not recognised formally in the community. Public transport was full fare even daily to and from the nursing home. Weighing the financial costs and the health benefits, it was an easy choice for me to elect to walk the eight-kilometre round-trip each day from the family home.”
The positive effects of the care he provided were significant and were frequently observed by other residents, relatives, nursing home staff and nurses, and medical experts. Even though the Parkinson's-type movement disorders and other physical aspects of Lewy Body Disease continued to tragically progress, the cognitive decline became increasingly difficult to discern, yet her personality was unchanging. She was comfortable and happy.
Specifically concerning was the progression of ‘physical aspects’. In late July 2019, an attending General Practitioner decided to note on Betty’s file as now to be regarded as receiving palliative care because of the continuing decline in her swallowing ability and an occasional feature of her breathing. David was told that he must be prepared for Betty’s imminent death and that he should not expect that her death within 14 days, from any beginning point from now on, would be a surprise. However, Betty's daily care pattern did not change by the nursing home or David, nor the medications she received. David instituted some small changes to feeding Betty her meals, and a minor physical therapy to help with those occasional features of her breathing when they appeared, after a discussion the next day with her specialist geriatrician.
The patient expert
"During my mum's whole experience from the first formal diagnosis of dementia, I was always in admiration of medical knowledge and dedication in dementia care and aged care," says David. "Whether from the Professor of geriatric medicine at the teaching hospital, the eye and skin specialists, speech pathologists and physiotherapists, registered nurses, general practitioners and care assistants in the family home and the nursing home, I was impressed by the medical knowledge and dedication on display. But I could not help wondering whether it was having its best potential effect for my Mum. If every person is different and every experience of dementia is different, what could this excellent medical knowledge and care achieve if it were tailored to those differences? I heard of the tremendous advances of tailored chemotherapy in cancer treatment. From years of observation, really the best outcome, especially through early palliative care of which I am now aware, is the partnership of the medical experts and the patient expert. I was the patient expert."
This notion of a patient expert is central to David’s thinking. Despite all the medical knowledge health professionals possess and can and do expertly apply, he argues that they can never have the full knowledge of the patient's condition and responses. Medical professionals spend very little time with each patient relative to potentially decades of close daily company and loving and careful interaction and observation. Their knowledge and understanding of their personality, their needs, joys, fears, likes, and dislikes. This is where the patient expert comes in: to partner and supplement the medical expertise and maintain the patient's quality of life. David particularly feels that the patient expert’s familiarity with the person in good health, and variation of presentations and behaviours long known to be consistent with their good health, enables the patient expert to identify at the earliest possible time signs of illness so that medical investigation and treatment can occur before an illness becomes serious and treatment is likely to be most effective and least stressful.
COVID-19 and visitor restrictions
COVID-19 and visitor restrictions broke this partnership of medical expert and patient expert that had achieved so much for Betty. When the pandemic broke out in Sydney, David was first told that his visitation hours would be restricted. Then, he was completely locked out of the aged care home from 27 March 2020. As he expected, citing two weeks as the focus of his concerns about her and his absence, and despite the aged care workers and health professionals' efforts, Betty's condition changed in the absence of his extended daily presence and care routine of the previous 3.5 years at the nursing home. Thirteen days later, David was summoned to urgently return to the nursing home on 9 April 2020; his mother was probably living her final hours: unconscious and breathing shallowly with oxygen; heartbeat irregular and colour poor. That sad prognosis was correct.
"In the small amount of time that was available, and because of her dementia, restricted movements, and loss of sight, all that could be arranged after 27 March 2020 was to use an additional mobile phone I hastily purchased so my Mum could hear my voice every day. Unfortunately, we could not converse this way. I had not been advised that she was not herself, or even unwell before being called to the nursing home to be with her in her last hours.”
“Sadly, she gave no sign she was aware of my presence on 9 April 2020. Could I only undo what she likely thought in her last two weeks of life after years of my daily care and affection ended suddenly? I wish I could assure her today, and every day forevermore, that I had not abandoned her and it was for not for anything she felt she may have done. I can’t.”
When COVID-19 first broke out and restrictions on visitation were put in place, David considered the option of taking his mother back to the family home. He dismissed this quickly as he knew that what he could provide as the "patient expert" was not enough without the "medical experts". Other practical difficulties could not be overcome quickly enough to ensure her safety.
"I never sensed, when the decision was made to exclude me, that I received any similar thought as the ‘patient expert’ in the partnership of her care, in the way that I had considered the role of the ‘medical experts’. It's a pity that I was excluded, and I believe this has a link with the fact that she died so quickly.”
David does not hold the nursing home to blame. He regards the death of his mother as a collateral COVID-19 death. "The circumstances that arose did not permit the transfer of my care regime, or as much of it that would have been necessary to sustain her until I could care for her again, in the time available and the confusion and wide disruption the COVID-19 outbreak produced in its early stages."
Nor did David argue then, or now, that there could never be circumstances when a total exclusion is necessary because of COVID-19; or any other disease outbreak for that matter.
What he has argued for, from the time of his first exclusion, is for assessment of the situation and needs of each resident and even the personal circumstances of the carer (perhaps living alone and having fewer community interactions than staff) when exclusions are being made. He wishes family carers were not labelled a ‘visitor’ automatically and feels it important not to overlook their previous role in daily care and the importance of the partnership of ‘medical experts’ and ‘patient expert’.
David also seeks a greater general awareness that untimely death does not appear on only one side of the decision about access or exclusion when dementia care and early palliative care are involved.
He sent a submission to the Royal Commission into Aged Care Quality and Safety on the subject of the ‘nursing home carer’ a year before the COVID-19 outbreak. He sent another one soon after Betty's death, drawing links to various aspects of the first submission and the value for the community and for nursing home residents of recognising the existence of ‘nursing home carers’ within the label of ‘visitors’. He also highlighted the benefits of the partnership between ‘medical experts’ and ‘patient expert’. He discussed his experience with multiple palliative care experts and has been invited to collaborate in research. The National Cabinet also noted the circumstances of Betty's death in the formulation of the draft aged care visitor access code.
Learning about palliative care
David wishes the importance of his role as a nursing home carer for his mother, and the ‘patient expert’ of the partnership, was either better understood or acknowledged, or both, so others will not have to experience a similar situation. Whether due to the COVID-19 pandemic broadly, or the panic of discovering his mother's health had suddenly deteriorated without his care and presence, David's invaluable contribution was undervalued. In reflection, David says, "Things do not always go to 'plan' to make for a smooth – or any – transition into end-of-life planning”.
Before this experience, David did not know what early palliative care was, and was unaware that the care he was providing to his mother was, in fact, a form of palliative care. He thought palliative care was limited to the process of actively dying when he was permitted to see Betty for the last time on 9 April 2020.
Now that he better understands palliative care, he says that it needs to be fully integrated into the care of people with dementia. He believes that palliative care if provided earlier, can considerably extend and improve the quality of life.
Relevant links supporting David’s experience
Dementia Australia and the University of Sydney 2020: ‘One day the support was gone. The mental health impact of COVID-19 on people living with dementia, their families and carers.’
ABC article 2020: Coronavirus lockdowns contributing to faster deterioration in dementia patients, research finds
The Australia New Zealand Society of Palliative Medicine (ANZSPM) has published guidelines to ensure visitor restrictions minimise harm and provide a flexible and proportionate response.
Palliative Care Australia's Palli8 plan to improve palliative care in aged care.

